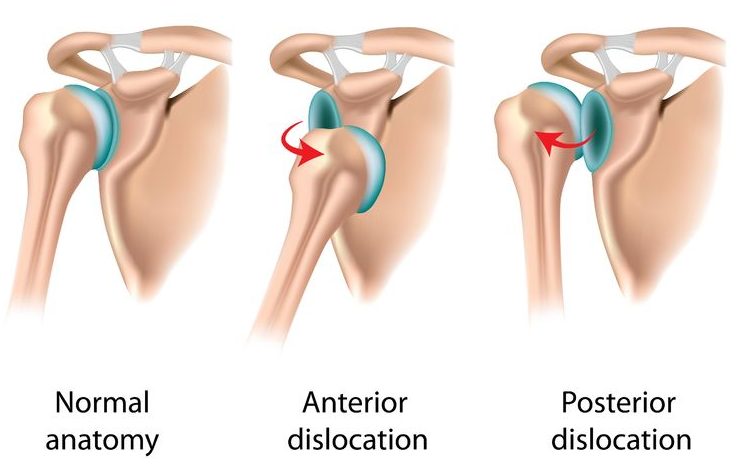
The shoulder is the most mobile joint in the body, but unfortunately this means that it is particularly prone to dislocation and instability.
How does the shoulder become unstable?
Although the shoulder is theoretically a ball and socket joint, the socket is extremely shallow. The joint therefore relies heavily on the ligaments and muscles for stability. The labrum is a fibrous ring around the edge of the glenoid (the shoulder socket) which deepens the socket, thus also helping to stabilise the shoulder joint. Shoulder instability is usually caused by an injury to the labrum and the shoulder ligaments. However instability may also be caused by weakness or poor coordination of the core stability muscles around the shoulder.
The spectrum of shoulder instability
Shoulder instability varies in severity. Recurrent shoulder disclocations occur when the ball comes right out of the socket and has to be put back by a doctor. Subluxations happen when the shoulder slips out, but then goes back by itself. The most mild form of shoulder instability may only cause pain, and sometimes clicking or the feeling that the shoulder just isn’t quite right.
How do you diagnose shoulder instability?
Clear-cut instability (repeated shoulder dislocations) is obvious. However more subtle instability may only be diagnosed by a specialist after careful examination. An MRI or CT scan is usually required in order to assess the extent of damage to the labrum and ligaments. Special dye may be injected into the joint in order to increase the accuracy of the scan.
How do you treat shoulder instability?
Physiotherapy is the first line of treatment if the underlying problem is weakness or poor coordination of the shoulder muscles and there is no physical damage to the joint. However if the labrum or ligaments are damaged, as is usually the case following trauma, then physiotherapy is generally ineffective.
Surgery is generally required when instability is caused by an injury to the labrum and ligaments. In the vast majority of cases, this can be performed as a keyhole operation. The damaged stuctures are repaired to the edge of the glenoid using extra strong sutures (stitches). These are passed around the labrum and fixed securely to the glenoid using special bone anchors which are drilled into the bone. This operation is known as an arthroscopic stabilisation.
Recovery and return to sport after stabilisation surgery
Weeks 0-6 after surgery: it is important to wear a sling in order to protect the repair. The sling can be removed for gentle passive exercises which your physiotherapist will show you, but the sling needs to be worn at all other times, including at night. Cardiovascular fitness can be maintained using a reclined static bike with low resistance so that you don’t use your arms or put any strain on the repair.
Weeks 7-12: the sling can be left off and you can start to use your arm for light activities such as eating, drinking and washing. However you shouldn’t lift anything heavier than a bag of sugar. Your shoulder is likely to be quite stiff at this stage, so physiotherapy is very important. This will start with some gentle stretches and then gradual strengthening exercises as your movement improves and the repair becomes stronger. You should be able to start some light running on the flat from around the 8-10 week mark.
Weeks 13-24: range of movement will continue to improve, but it is important to keep working on stretches as well as strengthening. The repair should now be strong enough to withstand increasing loads, though it is important to build this up gradually under the supervision of your physiotherapist. You should be able to return to sports as long as they don’t involve contact/impact or overhead use of the affected arm. However this very much depends on the speed of your recovery and the nature of your sport, so it is vital to discuss this with your surgeon and physiotherapist.
Weeks 24-52: maximum recovery typically takes 6 to 12 months from the time of surgery, so you should be nearly there. Contact or overhead sports may be reintroduced, provided you have regained a good range of movement with good strength and core stability. It is important to return to sport gradually and you must plan this with your surgeon and physiotherapist.